April wasn’t quite long enough this year for me to get the newsletter out in time – or something like that anyway. With thanks to Stephen Flanagan of the London PHE for his input into the measles textbox and Paul Gringras for help with the sleep series again. Jess has put together another superb article for her minor injuries series and I hope you find the links to the healthy weight clinics helpful for your patients locally. Click here for the April/May 2013 newsletter.
Tag Archives: trauma
Wrist injuries
Episode 4 and 5 of Jess Spedding’s minor injuries series are on the wrist.
Like in adults, the wrist is a very common location for injury. As an impulse to falling we stretch out our hands and arms to protect our head and torso, and hence the acronym FOOSH – fall on the outstretched hand, that you may come across in orthopaedic and Emergency Department documentation. The wrist is the most common upper limb fracture in adults, and is most common in children along with the supracondylar (see episode 2 of this series in December 2012 / January 2013). Whilst the supracondylar occurs in the 4-8y age group, wrist fractures which are typically distal radius fractures, can occur
at any age. Read more….
Episode 5 is on another wrist injury and one that must not be missed – scaphoid fractures. Read more….
February 2013 uploaded!
A timely reminder of an albeit old guideline on otitis media this month, continuation of our minor injuries series and introduction to a new series on sleep disorders. Also a link to a new Whipps “1st afebrile fit” guideline and a bit of background on hypospadias.
minor injuries series 3: ankle injury
Jess has written a lot of information about the assessment and management of ankle injuries which I have uploaded as a PDF here. I have put the Ottawa ankle rules below as a taster….
The wonderful thing about ankle injuries is that there is a reliable, commonly used, validated assessment of the injury that helps you to decide if an xray is indicated. This tool was developed by a group in Ottawa, Canada and for that reason bears the name “the Ottawa Ankle Rules” which are as follows:
Carry out an ankle xray (AP and lateral) if:
- The patient could not walk 4 paces immediately after the injury OR
- The patient cannot walk 4 paces now OR
- There is bony tenderness along the posterior aspect of the lateral OR
- medial malleolus from distal tip extending up 6cm
- (or xray the foot instead if base of 5th metatarsal tenderness)
You are very welcome to carry out an xray in those who do not fit these criteria if you are worried but there is a very low likelihood of there being a bony injury.
January 2013 – Happy New Year!
I was a bit overloaded in December and couldn’t manage to get a newsletter out. The nurses in my own ED noticed but I don’t think anyone else was particularly bothered! Hope the Christmas break went well for everyone. January 2013 brings some more on speech development, a reminder of the BTS 2008 guideline on cough, another plug for vitamin supplementation and part 2 of Jess Spedding’s minor injuries series. Do leave comments below.
Minor injuries part 2
With thanks to Dr Jess Spedding for the continuation of her minor injuries series….
Minor Injuries Series, part 2: The Elbow Xray and Supracondylar fracture:
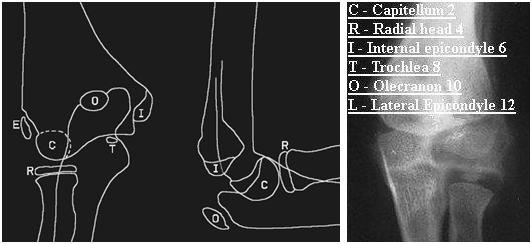
The elbow xray typically strikes fear into the heart of clinicians as there are so many centres of ossification which appear at different stages of a
child’s development and can quite easily be mistaken for bony injury. Remember that the smooth rounded appearance of a centre of ossification does not often mimic the typically sharp edges of a new fracture fragment, but even saying this, distinction can be very difficult. If you have the CRITOL (or CRITOE) acronym in your mind, it will help you to interpret the xray with a sensible approach. The image below highlights each of the six ossification centres with the typical age of the child when each centre appears:
Note: Lateral / External epicondyle are interchangeable terms, giving either CRITOL or CRITOE
Work through in order the centres of ossification – each may appear at slightly different ages in different children, but the sequence in which they
appear should always be C,R,I,T,O,L. For example in a 6 year old you would not expect the lateral condyle to have appeared yet, so if there is a bony fragment at that site, it is suggestive of a fracture.
Supracondylar Fractures:
The supracondylar fracture (of the distal humerus) is the most common upper limb fracture in young school age children. It presents almost always as
a FOOSH (fall on the outstretched hand). They are likely to be in a lot of pain, and may need strong analgesia and immobilisation (with a splint or
sling) before assessment is possible. (A good example of a strong, rapid acting, well tolerated analgesic that can be used in the Emergency Department is intranasal diamorhpine, which is made up with saline into a small volume of fluid and then given as nose drops with a syringe.)
You may well see bruising and swelling around the elbow, with tenderness around the distal humerus, but remember to check the whole limb including
clavicle (and the whole of their body if the mechanism of injury could have caused other serious injuries!)
The elbow contains numerous important neurovascular structures – your assessment must document presence of radial pulse, capillary refill time in
fingertips and function of ulnar, median and radial nerves (not possible formally in younger children, so watch to see if they will hold a toy or parents hand
and be suspicious if the xray shows a displaced fracture). Any concerns about neurovascular compromise require the fracture to be urgently reduced, either by the Emergency Department team or referral to Orthopaedics. This initial reduction is to relieve mechanical pressure of displaced bony fragments on the
neurovascular structures and will not provide the stability required for neatly aligned healing, so a trip to theatre for fixation will happen soon after.
A common classification system for supracondylar fractures is the Gartland classification. In this there are three categories of supracondylar fractures based on their radiological appearance on the lateral elbow view:
1: undisplaced – recognised as clinical suspicion plus xray evidence of fluid in the elbow joint elbow (as demonstrated by a raised anterior fat pad or
the presence of a posterior fat pad) and possibly loss of anterior humeral line (normal is when line along anterior humerus intersects middle third of
capitellum)

2. visible fracture which is hinging on the posterior edge

3. totally displaced
Type 1 can usually be managed conservatively with an above elbow cast and sling, whilst 2 and 3 require operative fixation.
All should be followed up by Orthopaedics in fracture clinic – typical progress is evidence of union at 4 weeks, and then the patient is encouraged to
gradually do away with the sling, to allow mobilisation without too much discomfort.
A rare but debilitating late complication of supracondylar fractures is Volkmann’s ischaemic contracture (when the brachial artery is damaged and months later the patient develops clawing of the thumb and fingers and forearm wasting).
November 2012 published!
The common assessment framework triangle for assessing children in need this month with some tips on how to press the right buttons with children’s social care referrals. Also a bit on stabilisation and transfer for the ED teams, a reminder not to use 0.18% saline and the start of a minor injuries series. Talipes for the GPs and paediatricians among you.
Minor injuries introduction
Minor injuries Series: Episode 1 with thanks to Dr Jessica Spedding, PEM trainee, Royal London Hospital, UK
Introduction to minor injuries:
Minor injuries in children are common and mostly self limiting soft tissue injuries that heal with time. Some injuries are particular to paediatrics (pulled elbow) and others are simply much more common in children than adults (supracondylar fracture). Another consideration specific to children is consideration of growth plate involvement, which if does not heal in a good position could lead to asymmetry and growth problems. Injuries involving the growth plate are graded as Salter-Harris 1,2,3,4, or 5 and they will be discussed in more detail in a future episode of this minor injuries series.
Your assessment:
You need a systematic approach that assesses for important injuries that need specific management. Your
assessment must always include consideration of non accidental injury (NAI). A sensible approach would include:
– Is the mechanism of injury described consistent with the injury sustained?
– Has the child reached the appropriate stage of development to have sustained the injury in the way described?
– Is there any delay in presentation?
– Has the child (or siblings) presented numerous times before with injuries?
– There is an excellent set of pamphlets that give evidence based guidance on when injuries point to abuse – go to www.core-info.co.uk or look out for the summaries on Paediatric Pearls
Upper limb injuries:
You may have come across the acronym FOOSH. This is a Fall On the Out-Stretched Hand. This mechanism is the natural response to a fall – in order to protect our head and trunk, the reflex is to put our arms out to break our fall. This mechanism causes a number of different injuries, each more prevalent in different age groups (but common in other age groups too). Roughly speaking these could be sequenced as follows:
Age 1-3: distal radius fracture (usually greenstick or torus) or middle third clavicle fracture
Age 4-8: supracondylar fracture (varying degrees of severity, some of which require operative fixation)
Age 9-adulthood: distal radius fracture or scaphoid fracture
However one must still examine unclothed the whole limb to be sure that all sites of injury have been located. In the upper limb this would be from
fingers to shoulder, clavicle and possibly neck, in the lower limb this would be from toes to hips but also checking the pelvis and lower spine.
The first chapter in this series looks at a common elbow problem:
Pulled elbow: (see also http://www.paediatricpearls.co.uk/2012/02/pulled-elbow/)
 Proper name – radial head subluxation, mechanism is usually a sudden pulling of the child by their hand (such as to stop them running into the road or swinging a child in play), child presents having cried initially, but soon settles but refuses to use the arm, holding it slightly flexed at the elbow with the arm by their side. When you go to assess them they have no swelling or bruising or distal neurovascular compromise, but are very apprehensive about you trying to bend or pronate/supinate the elbow. In up to half of cases there may not be a “pull” mechanism in which case be more cautious in assuming the diagnosis. Don’t forget a clavicle fracture may present this way. If you feel sure the diagnosis is pulled elbow, attempt a reduction as follows:
Proper name – radial head subluxation, mechanism is usually a sudden pulling of the child by their hand (such as to stop them running into the road or swinging a child in play), child presents having cried initially, but soon settles but refuses to use the arm, holding it slightly flexed at the elbow with the arm by their side. When you go to assess them they have no swelling or bruising or distal neurovascular compromise, but are very apprehensive about you trying to bend or pronate/supinate the elbow. In up to half of cases there may not be a “pull” mechanism in which case be more cautious in assuming the diagnosis. Don’t forget a clavicle fracture may present this way. If you feel sure the diagnosis is pulled elbow, attempt a reduction as follows:
 Hold their hand as though you were going to shake hands, with your other hand gently cupping underneath the elbow, with elbow partially flexed, then firmly pronate (rotate to palm up position). You should feel the clunk of a reduction, but if not, try a firm supination (back to palm down position). Ideally do this half an hour after some analgesia. If you do not feel a clunk it is probably not reduced but either way stop after two attempts, and then allow the child to be somewhere relaxing and ask their parent to let you know if they start playing – if reduced most will soon realise the pain with movement has gone and start playing normally within a few minutes. If not reassess and consider a differential diagnosis which may include referral for xray.
Hold their hand as though you were going to shake hands, with your other hand gently cupping underneath the elbow, with elbow partially flexed, then firmly pronate (rotate to palm up position). You should feel the clunk of a reduction, but if not, try a firm supination (back to palm down position). Ideally do this half an hour after some analgesia. If you do not feel a clunk it is probably not reduced but either way stop after two attempts, and then allow the child to be somewhere relaxing and ask their parent to let you know if they start playing – if reduced most will soon realise the pain with movement has gone and start playing normally within a few minutes. If not reassess and consider a differential diagnosis which may include referral for xray.
October 2012 ready to go!
Coins, magnets and batteries on the menu this month as well as some more cows milk protein allergy resources. A reminder about child developmental milestones courtesy of one of our medical students and NICE on headaches. Do leave comments!
Foreign body ingestion
The information for this topic is taken from a recent comprehensive review (August 2012) that appeared in www.UpToDate.com. Bartshealth employees can access the full text via a link from the intranet.
Ingested foreign bodies (UptoDate.com article, August 2012)
Coins — Coins are by far the most common foreign body ingested by children. Approximately two-thirds of ingested coins are in the stomach by the time of x-ray but those that lodge in the oesophagus for 24 hours after ingestion may need to be removed endoscopically as only 20-30% of these will pass into the stomach on their own. Coins that reach the stomach can be managed expectantly, and most will be passed within one to two weeks. A child who develops any signs or symptoms of obstruction, abdominal pain, vomiting, or fever, needs to come back to the ED urgently.
Button batteries — ingestions of “button” batteries are increasing and are associated with significant morbidity. Animal studies have demonstrated mucosal necrosis within one hour of ingestion and ulceration within two hours, with perforation as early as eight hours after ingestion. It may be difficult to differentiate between a disk battery and a coin on a radiograph. This distinction is most important when the foreign body is in the oesophagus, since batteries require immediate removal whereas coins may not.
Magnets — also increasing. Many of the children with complications from multiple magnet ingestion had underlying developmental delay or autism. In one case, an older child inadvertently swallowed these magnets while using them to imitate a pierced tongue. Two or more strong magnets, especially if ingested at different times, may attract across layers of bowel leading to pressure necrosis, fistula, volvulus, perforation, infection, or obstruction. Radiographs of the neck and abdomen should be performed, including a lateral view. X-rays cannot usually determine whether bowel wall is compressed between the magnets, although the finding of magnets that appear to be stacked but are slightly separated is suggestive. Management depends on the number, location and type of magnets, and on the timing of the ingestion. Ingestion of a single magnet can generally be managed conservatively with serial radiographs while multiple magnets need removing. Laxatives may help with faster bowel emptying if they are not in a place easily accessible with the endoscope.
References at www.uptodate.com.